Written Qualifying Exam: Types Of Test Questions
The ABO lists 7 aspects of ophthalmic knowledge that the written qualifying exam aims to assess. Understanding what they are trying to test may also provide insight into the types of questions that you might expect to see. Many of these aspects are interdependent. Again, as a disclaimer, I am not reproducing any example test questions from memory; any similarities to actual test questions is purely coincidental (I do not write questions for the WQE, and it’s been several years since I took the test). Also, the exposition on these topics is purely my personal opinion and not directly from the ABO.
Recall of Information
If you ask around, I think most people who have taken the WQE will say that the recall questions are far more challenging than the ones on the OKAP. The reason is, most of the questions are not 1-step questions, such as: “Which one of these muscles is not innervated by the oculomotor nerve?” Instead, most of the questions are multi-step questions, where the recall of information is part of what you need to answer the question. Recall may also be bundled in with other questions, where you will use recall to identify the disease process and then answer some other question about the disease.
Example Question
Image from University of Iowa, EyeRounds
A 34-year-old pregnant woman with a past medical history significant for hypercholesterolemia and asthma presents for evaluation after being hit in the eye by her 2-year-old. Her slit-lamp exam is shown. Her visual acuity is 20/40, and has an intraocular pressure of 33 mmHg. What of the following would be the best option for initial treatment?
A. Brimonidine (Alphagan P)
B. Dorzolamide (Trusopt)
C. Timolol (Timoptic)
D. Travoprost (Travatan Z)
So this question (which may be too easy) really tests several pieces of recall – what medications are not safe to use in pregnancy, what medications may not be ideal in asthmatics, and what medications might not be ideal in people with high cholesterol.
(The correct answer is A – carbonic anhydrase inhibitors and prostaglandin analogues are contraindicated in pregnancy, and nonspecific beta-blockers such as timolol are relatively contraindicated in asthmatics, which makes brimonidine the best option.)
Understanding and Application of Basic Knowledge
These understanding/application questions may be similar to the level 2 and 3 questions on the OKAP. I may be off on the interpretation of this concept, but I think the idea is that some test questions will see if you can take the “next step” and apply the recall knowledge you have to a clinical situation.
Example Question
A 26-year-old female presents to your office complaining of recent-onset vision loss in the left eye associated pain, worse when looking up. Her vision is 20/15 in the right eye and 20/60 in the left eye. She has a left relative afferent pupillary defect, and a dense central scotoma in the left eye on visual field testing. Her eye exam is otherwise normal. Which of the following is the most appropriate next step in management?
A. Intravenous methylprednisolone
B. Lumbar puncture with opening pressure
C. MRI brain with and without contrast
D. Oral prednisone
There needs to be some basic recall, such that based on the vignette you instantly can recognize the condition being described (in this case, left retrobulbar optic neuritis). Additionally, you need to have at least a basic understanding of the management of optic neuritis (in this case, the conclusions of the Optic Neuritis Treatment Trial), to know how to best answer this question and to apply those results to this patient.
(The correct answer is C – the Optic Neuritis Treatment Trial concluded that oral prednisone treatment in the setting of typical retrobulbar optic neuritis is contraindicated, because it dramatically increased the risk for future recurrence of optic neuritis. The ONTT also found that IV steroid treatment (their protocol was IV methylprednisolone 250 mg every 6 hours for 3 days followed by oral prednisone for 11 days for a total of 14 days of steroid treatment) was only indicated in patients who had 2 or more T2/FLAIR hyperintense lesions on their MRI; the treatment, while it sped up recovery, did not have any statistical benefit on final visual acuity outcomes. However, in patients with 2 or more lesions on their MRI, IV steroid treatment decreased their risk for MS progression by 50% over the next 2 years. Therefore, all patients with typical retrobulbar optic neuritis need to obtain an MRI of the brain with and without contrast to assess their risk for progression to MS, and to determine whether they require IV steroid therapy as a result of their MRI findings. A lumbar puncture is not required for the diagnosis of optic neuritis, but may be ordered in atypical cases.)
Relation of Pathogenesis to Disease Process
One of the aspects that we often miss or forget in medicine is how our understanding of a disease’s pathogenesis can guide us logically to refine our differential diagnoses, predicting clinical behavior of a disease, or develop effective treatments. While a great deal of our clinical practice centers around more practical and pragmatic concerns than recalling the higher conceptual ideas we may have glossed over in residency, the WQE will still test us over some of these key concepts to make sure that we have an adequate basis of knowledge. Having that fundamental understanding of ocular disease not only can help you accurately identify diseases and treatments, but also help you counsel your patients and educate them about their condition (which, in turn, may help improve compliance with your recommendations).
Example Question
Which of the following corneal findings may be a complication of diabetes?
A. Guttata
B. Central thinning
C. Enlarged nerves
D. Recurrent erosions
This question really builds upon the principles of the previous aspects – there is some basic recall required (as some of these facts may be memorized). There is some application of that knowledge to arrive at some of the answer choices. Finally, an understanding of the pathogenesis of diabetic changes within the cornea is very helpful in arriving at the correct answer.
(The correct answer is D – thickened basement membranes (a common pathologic feature of diabetes) within the corneal epithelial basement membrane leads to a decrease in the number of hemidesmosomes, which can cause recurrent epithelial erosions. Excess glucose drives the sorbitol pathway, which leads to the accumulation of sorbitol within various ocular tissues. Within the cornea, deposits of polyols such as sorbitol in the corneal epithelium and endothelium lead to dysfunction of those layers. This results in decreased corneal sensitivity (hypoesthesia). Over time, the hypoesthesia can result in neurotrophic keratopathy, which causes irregular astigmatism. However, this does not result in enlarged corneal nerves, which is seen in multiple endocrine neoplasia type 2B, keratoconus, leprosy, Refsum disease, neurofibromatosis type 1, acanthamoeba infection, and Fuchs endothelial corneal dystrophy. Corneal guttae are not a specific finding in diabetics. Corneal endothelial dysfunction results in an increase in stromal hydration, not decrease; therefore there can be an increase in corneal thickness in diabetics.)
Evaluation of Clinical Data
Honestly, I interpreted this aspect in a couple of different ways. First, I think this refers to the method by which we take all of the clinical data (history, exam, ancillary tests, diagnostic tests, etc.) and synthesize it into a meaningful differential diagnosis. Second, I think it also refers to the interpretation of said ancillary tests. As such, I think there are probably going to be some test questions that require you to be able to accurately interpret the results of an ancillary test (typically a visual field, OCT, or fluorescein angiography; simple ERG patterns are likely fair game as well).
Example Question
Image from: University of Stanford, Department of Ophthalmology. Posted by tcooper. Case first described in: Newman, NJ. Treatment of hereditary optic neuropathies. Nat Rev Neurol. 2012:8;545–556.
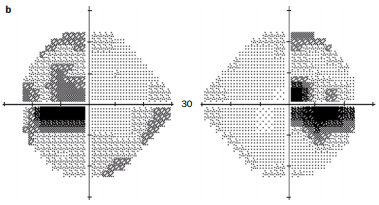
Which of the following conditions may cause the visual field defects shown?
A. Hereditary optic neuropathy
B. Ischemic optic neuropathy
C. Paraneoplastic optic neuropathy
D. Radiation optic neuropathy
In this question, you have to interpret the visual field - is it a bitemporal hemianopia, enlarged blind spots, cecocentral scotomas, etc.? Once you decide what you think might be the correct visual field pattern, then you have to recall what the differential diagnosis would be for that pattern.
(The correct answer is A - this is visual field represents bilateral cecocentral scotomas, though an early bitemporal hemianopia could also be considered. As such, hereditary optic neuropathies such as Leber's hereditary optic neuropathy and OPA1-associated optic atrophy should be considered. Additionally, nutritional deficiency optic neuropathies, such as vitamin B12 deficiency, may also cause this visual field pattern. Other considerations include toxic optic neuropathies (such as ethambutol, which can affect the chiasm), bilateral optic neuritis, optic chiasmitis, and chiasmal compression. Ischemic optic neuropathies typically cause altitudinal defects (NAION) or dense central scotomas (severe NAION, AAION, or PION). Paraneoplastic and radiation optic neuropathies typically cause dense central scotomas.)
Utilization of Diagnostic and Therapeutic Procedures
As you might imagine, being able to correctly identify pathology and recognize the patterns of disease is only one step in the process to being an excellent ophthalmologist. Recognizing the appropriate tests to order for diagnosis and correctly managing the disease are just as important. Test questions involving this aspect of ophthalmology will often present a clinical vignette from which you have to recognize the appropriate disease, then decide what would be the appropriate management.
Example Question
A 4-year-old presents for evaluation. The macular OCT is shown below. What is the next appropriate step in management?
Image from: Goetz K, Vislisel JM, Raecker ME, Goins KM. Congenital Aniridia. March 10, 2015; Available from: http://EyeRounds.org/cases/211-Aniridia.htm
A. Visual evoked potentials
B. Complete blood count
C. Abdominal ultrasound
D. Urine catecholamines
(The answer is D - although the image is taken from a case of congenital aniridia, the test question does not specify any details that would indicate the exact pathology of the condition. In cases of mild albinism, a VEP may be helpful for diagnosis, because the temporal fibers of each optic nerve also decussate (only nasal fibers cross in normal individuals), resulting in asymmetric VEPs. In certain special cases of albinism (Chediak-Higachi syndrome being most notable), patients may have decreased platelets, which would make obtaining a complete blood count helpful. Hermansky-Pudlak syndrome, another special variant of albinism, has platelet dysfunction without decreased platelet counts. An abdominal ultrasound is also helpful in the workup of aniridia, as there is an association with Wilms tumor, especially in cases of sporadic aniridia.)
Anticipation and Recognition of Complications
In both clinical and surgical practice, it is crucial for us to anticipate potential complications, as well as recognize them as they occur, so that appropriate steps can be taken to minimize their long-term effects.
Example Question
A 45-year-old with 45 prism diopters of alternating esotropia undergoes bilateral medial rectus recession surgery. Which of the following would require prompt attention?
A. Severe subconjunctival hemorrhage and conjunctivochalasis
B. Severe ocular pain
C. 10 prism diopters of exotropia at post-operative day 1
D. Limited adduction at post-operative day 8
(The answer is D - while conjunctivochalasis can lead to corneal delle which would require aggressive lubrication and sometimes surgical intervention, significantly limited adduction after medial rectus surgery may signify a slipped muscle, which requires urgent exploration to try and retrieve the lost muscle. Pain may be normal in the first few days of the post-operative period, and slight overcorrection is possible during the first post-operative days.)
Ethics of Ophthalmic Practice
To be honest, I don't know what kind of questions would best fit in this category. Ethical practice is an important aspect of clinical practice, and sadly has to be emphasized because there are the rare "bad apples" that taint the perception of medical practice. However, I personally do not recall specific questions about ethical situations on the test (for what that's worth). It's more likely that you will be asked about appropriate management or counseling, and perhaps recognizing the generally accepted workup and treatment order of least invasive to most invasive, ruling out life-threatening and sight-threatening disease, and conservative management before elective surgery (with the notable exception of knowing when to decisively act on emergency surgery). Because I don't want to lead you down the wrong path by making up a sample question that may be completely wrong, I will leave this section questionless. For those who have taken the written exam more recently, please leave a comment or e-mail us if you have a good example of test questions that might evaluate this aspect!
In subsequent posts on this topic, I will discuss the essential topics that should be reviewed when studying for the WQE, resources and tools I found helpful when preparing for the WQE, developing a reasonable study schedule, and test-taking strategies/tips for the WQE.
Was this a helpful overview? Do you have helpful hints about the test that you'd like to share? Contact me and I'll add it to the article!