Left Horner syndrome.
Image credit: American Academy of Ophthalmology. Used with permission for educational purposes.
Horner syndrome describes the constellation of findings associated with a lesion affecting the oculosympathetic pathway. Clinically, ipsilateral miosis, ptosis, and anhidrosis form the classic triad, with other features potentially being present.
Without getting into too much detail about the sympathetic pathways and differential diagnosis of Horner syndrome (those will be covered in other articles), I will attempt to highlight the 3 pharmaceutical agents used in the diagnosis of Horner syndrome, discuss the tests, and point out the key ideas that often find themselves in tests.
Caveat: Because of the general unavailability of some of these drugs (namely cocaine and hydroxyamphetamine) and the relatively lower cost/availability of neuroimaging, these drugs may not be available to your local neuro-ophthalmologist. There are evolving discussions about navigating the challenges of diagnosis given these limitations (1, 2). Despite these changes to practical clinical evaluation, it remains clinically important to understand the pharmacologic principles involved in the diagnosis of Horner syndrome.
Classification
The pharmacologic diagnosis of Horner syndrome can be broken into two major categories:
Confirming the diagnosis of Horner syndrome
Cocaine
Apraclonidine
Localizing Horner syndrome to preganglionic (1st-/2nd-order) or postganglionic (3rd-order) neuron
Hydroxyamphetamine
Diagnostic Drops
Cocaine
The cocaine test for Horner syndrome is often tested in board exam/OKAP settings, most likely because of its understood mechanism of action, its contribution to the understanding/diagnosis of Horner syndrome, and somewhat counterintuitive testing results.
From a practical standpoint, relatively few clinics have cocaine available for Horner syndrome testing, largely due to the unavailability, high cost with no reimbursement, and security requirements for storage. So although cocaine is discussed from a historical context, we unfortunately have to also learn the details of this test so that you can easily answer any questions that might pop up on a test. Just don’t be surprised if you can’t find any doctors who can do a cocaine test for Horner (it might not be necessary anyways).
Mechanism of action: blocks the reuptake of norepinephrine into presynaptic neurons at the synapse of postganglionic sympathetic nerves and muscle (in eye drops, synapse of long ciliary nerves and iris dilator muscle).
Cocaine test for Horner syndrome (19).
A. Before drops administered (suspected right Horner syndrome).
B. After drops administered. Note that there is some pupil dilation in the right eye, but the amount of anisocoria is ≥1 mm.
Image credit: Kanagalingam S, Miller NR. Eye Brain 2015;7:35-46. Available online. Used under the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
Test (3, 4):
Measure pupil size of both eyes
Instill 1 drop of cocaine (4% or 10%) in each eye, wait 5 minutes, then an additional 1 drop of cocaine in each eye
Wait 40-60 minutes
Remeasure pupil size of both eyes
Results:
No reaction after 60 minutes: put one more drop of cocaine, wait another 30 minutes
Pupillary inequality ≥ 1.0 mm: positive test for Horner syndrome (the greater the inequality, the more accurate it gets)
Pupillary inequality < 1.0 mm: negative test for Horner syndrome
Considerations:
Urine drug test for cocaine will be positive for a few days after testing (5)
Apraclonidine
Apraclonidine is the most readily available drug used for confirming Horner syndrome. Because this drop is often available in comprehensive ophthalmology clinics for other uses (it lowers IOP and may be used as a pre- or post-treatment for in-office procedures), knowing how to administer this test may be helpful for confirming Horner syndrome, especially if neuro-ophthalmology is not readily available.
Mechanism of action: α2-adrenergic agonist, weak α1-adrenergic agonist; in Horner syndrome, sympathetic denervation hypersensitivity of α1-receptors occurs within the pupillary dilator muscle.
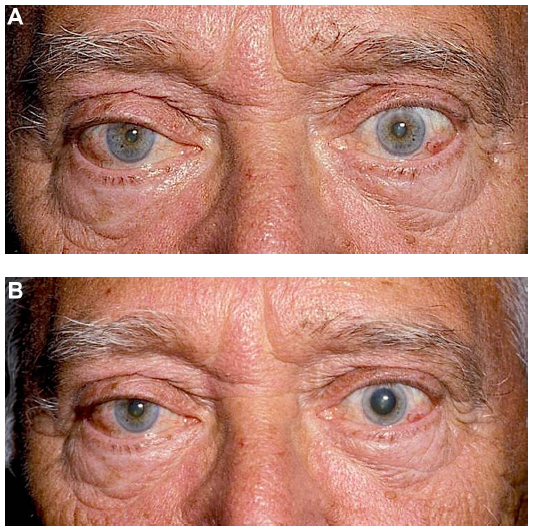
Apraclonidine test for Horner syndrome (19).
A. Before drops administered (suspected left Horner syndrome).
B. After drops administered. Note the slight “reversal of anisocoria” in the left eye and the resolution of ptosis.
Image credit: Kanagalingam S, Miller NR. Eye Brain 2015;7:35-46. Available online. Used under the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
Test (6-13):
Note anisocoria (which pupil is small, which pupil is larger)
Instill 1 drop of apraclonidine (0.5% or 1%) in each eye
Wait 40-60 minutes (effects can be quicker)
Re-evaluate anisocoria
Results:
The smaller pupil dilates, normal pupil stays the same (reversal of anisocoria): positive test for Horner syndrome
No change to pupils: negative test for Horner syndrome
Considerations:
Denervation must be present long enough for receptor upregulation to have occurred (14)
Positive tests have been noted within hours of a carotid dissection but the onset of denervation sensitivity are variable (15)
False negatives can occur in the setting of acute Horner syndrome or in long-standing cases if strict “reversal of anisocoria” criteria used (16, 17)
Apraclonidine has limited use in pediatric Horner syndrome due to the risk of CNS and respiratory depression (18)
Hydroxyamphetamine
Hydroxyamphetamine remains a useful tool for localization of the lesion once a diagnosis of Horner syndrome has been confirmed (20). However, it is limited by accessibility and some considerations detailed below. Since it’s still tested (and important to understand from a mechanistic and historical perspective), you still need to know how it works and what it does.
Mechanism of action: increases the release of norepinephrine from the presynaptic neuron (21). In intact presynaptic (3rd order, postganglionic) neurons, this results in pupil dilation; if this neuron is not intact, the pupil does not dilate.
Hydroxyamphetamine test for Horner syndrome (19, 21).
A. Before drops administered (suspected right Horner syndrome).
B. After drops administered. Note the dilation of both pupils. This indicates an intact 3rd-order, postganglionic neuron and localizes the lesion to the 1st-order (central) or 2nd-order (preganglionic) neuron.
Image credit: Modified from clinical images courtesy of Lanning B. Kline, M.D. American Academy of Ophthalmology. Used with permission for educational purposes.
Test (21-25):
Note anisocoria (which pupil is small, which pupil is larger)
Instill 1 drop of hydroxyamphetamine (1%) in each eye
Wait 45-60 minutes
Re-evaluate anisocoria
Results:
In patients with normal pupils, there is a symmetric 2 mm dilation of each pupil (anisocoria remains) (22).
In patients with Horner syndrome, the reaction is based on whether or not there is an intact 3rd-order (postganglionic) neuron (23):
Both pupils dilate: intact 3rd-order neuron (localizes to 1st- or 2nd-order neuron)
Only non-Horner pupil dilates: not intact 3rd-order neuron (localizes to 3rd-order neuron)
Considerations:
Cocaine interferes with the uptake and efficacy of hydroxyamphetaine; as such, if cocaine is used for confirming the diagnosis, at least 72 hours must pass before hydroxyamphetamine testing is done (26).
In cases where there is concern for rapid diagnosis and localization (such as in carotid dissection), don’t delay neuroimaging for the hydroxyamphetamine test!
In acute Horner syndrome, hydroxyamphetamine testing may produce a false-negative result during the first week after injury (27-28).
Video Lecture
Dr. Andrew Lee is a highly-regarded neuro-ophthalmologist and a phenomenal educator. He has made some short lecture videos on neuro-ophthalmology available on YouTube!
Video credit: Lee AG. Pharmacologic Testing for Horners. Video. YouTube. Available online. Accessed 02-27-2019.
Further Reading
Basic and Clinical Science Course, Section 5. Neuro-Ophthalmology. San Fransisco: American Academy of Ophthalmology; 2018-2019:257-262.
Mughal M, Longmuir R. Current pharmacologic testing for Horner syndrome. Curr Neurol Neurosci Rep 2009;9:384-389.
Maloney WF, Younge BR, Moyer NJ. Evaluation of the causes and accuracy of pharmacologic localization in Horner’s syndrome. Am J Ophthalmol 1980;90:394-402.
Reede DL, Garcon E, Smoker WR, Kardon R. Horner’s syndrome: clinical and radiographic evaluation. Neuroimaging Clin N Am 2008;18:369-385.
References
Kardon R. Are we ready to replace cocaine with apraclonidine in the pharmacologic diagnosis of Horner syndrome? J Neuroophthalmol 2005;25:69-70.
Trobe JD. The evaluation of Horner syndrome. J Neuroophthalmol 2010;30:1-2.
Van der Wield HL, Van Gijn J. The diagnosis of Horner’s syndrome. Use and limitations of the cocaine test. J Neurol Sci 1986;73:311-316.
Kardon RH, Denison CE, Brown CK, Thompson HS. Critical evaluation of the cocaine test in the diagnosis of Horner’s syndrome. Arch Ophthalmol 1990;108:384-387.
Jacobson DM, Berg R, Grinstead GF, et al. Duration of positive urine for cocaine metabolite after ophthalmic administration: implications for testing patients with suspected Horner syndrome using ophthalmic cocaine. Am J Ophthalmol 2001;131:742-747.
Koc F, Kavuncu S, Kansu T, et al. The sensitivity and specificity of 0.5% apraclonidine in the diagnosis of oculosympathetic paresis. Br J Ophthalmology 2005;89:1442-1444.
Martin TJ. Horner’s syndrome, Pseudo-Horner’s syndrome, and simple anisocoria. Curr Neurol Neurosci Rep 2007;7:397-406.
Lebas M, Seror J, Debroucker T. Positive apraclonidine test 36 hours after acute onset of Horner synndrome in dorsolateral pontomedullary stroke. J Neuroophthalmol 2010;30:12-17.
Peterson JD, Bilyk JR, Sergott RC. But it’s not all there. Surv Ophthalmol 2013;58:492-499.
Cambron M, Maertens H, Crevits L. Apraclonidine and my pupil. Clin Auton Res 2011;21:347-351.
Morales J, Brown SM, Abdul-Rahim AS, Crosson CE. Ocular effects of apraclonidine in Horner syndrome. Arch Ophthalmol 2000;118:951-954.
Brown SM, Aouchiche R, Freedman KA. The utility of 0.5% apraclonidine in the diagnosis of Horner syndrome. Arch Ophthalmol 2003;121:1201-1203.
Freedman KA, Brown SM. Topical apraclonidine in the diagnosis of suspected Horner syndrome. J Neuroophthalmol 2005;25:83-85.
Bohnsack BL, Parker JW. Positive apraclonidine test within two weeks of onset of Horner syndrome caused by carotid artery dissection. J Neuro-ophthalmol 2008;28:235-236.
Cooper-Knock J, Pepper I, Hodgson T, et al. Early diagnosis of Horner syndrome using topical apraclonidine. J Neuroophthalmol 2011;31:214-216.
Kawasaki A, Borruat FX. False negative apraclonidine test in two patients with Horner syndrome. Klin Monatsbl Augenheilkd 2008;225:520-522.
Dewan MA, Harrison AR, Lee MS. False-negative apraclonidine testing in acute Horner syndrome. Can J Ophthalmol 2009;44:109-110.
Bacal DA, Manche EE. The role of apraclondine in the diagnosis of Horner syndrome in pediatric patients. Arch Ophthalmol 2004;122:276-279.
Kanagalingam S, Miller NR. Horner syndrome: clinical perspectives. Eye Brain 2015;7:35-46. Available online.
Sadaka A, Schockman SL, Golnik KC. Evaluation of Horner syndrome in the MRI era. J Neuroophthalmol 2017;37:268-272.
Thompson HS, Mensher JH. Adrenergic mydriasis in Horner’s syndrome. Am J Ophthalmol 1971;72:472-480.
Cremer SA, Thompson HS, Digre KB, et al. Hydroxyamphetamine mydriasis in normal subjects. Am J Ophthalmol 1990;110:66-70.
Cremer SA, Thompson HS, Digre KB, et al. Hydroxyamphetamine mydriasis in Horner’s syndrome. Am J Ophthalmol 1990;110:71-76.
Mindel JS. Hydroxyamphetamine test in Horner’s syndrome (letter). Am J Ophthalmol 1975;79:523-525.
Thompson HS, Mensher JH. Hydroxyamphetamine test in Horner’s syndrome (reply). Am J Ophthalmol 1975;79:525-526.
Wilhelm H, Welhelm B, Kriegbaum C. Interaction of the indirectly acting topical sympathomimetics cocaine and pholegrine. Ger J Ophthalmol 1996;5:168-70.
Moster ML, Galiani D, Garfinkle W. False negative hydroxyamphetamine test in Horner syndrome caused by acute internal carotid artery dissection. J Neuro-ophthalmol 2003;23:22-23.
Donahue SP, Lavin PJM, Digre K. False-negative hydroxyamphetamine (Paredrine) test in acute Horner’s syndrome. Am J Ophthalmol 1996;122:900-901.
Do you have any tips on how to remember the pharmacologic testing for Horner syndrome? Leave a comment or contact us!