Prisms, like double vision, seem to be pretty dreaded by most people (aside from strabismus specialists and optics fans). For testing purposes and clinical applications, we thankfully don't have to know a ton of things about prisms apart from the essential applications within our clinics. Hopefully this will help you understand the principles of prisms better so that you can use them effectively in clinic as well as answer any test questions that might pop up!
The Prism Diopter
Prisms bend light (i.e., change the direction of a light ray). We use the unit prism diopter (Δ) to quantify how much a prism will bend light. This is different from the diopters used to describe the refractive power of a lens (D) - don't get these two things confused!
A prism diopter is the distance an image is shifted by the prism (in cm) at a distance of 1 m (or 100 cm) away from the prism.
(Illustration developed by Edmond H. Thall, MD, and Kevin M. Miller, MD, and rendered by C. H. Wooley.)
Image credit: American Academy of Ophthalmology. Used with permission.
Example Question
A prism is placed in front of an object. The resulting image is displaced 10 cm at 2 m. What is the power of the prism, in prism diopters?
A. 5 Δ
B. 10 Δ
C. 15 Δ
D. 20 Δ
Answer: A. The prism displaces the image 10 cm at 2 m, or 5 cm at 1 m (10 cm/2).
How To Hold Prisms In Clinic
When you're using prisms, it matters if the prism you're holding is made of glass or plastic. Glass prisms, like the ones in a trial lens set, should be held parallel to the iris regardless of what direction the eye is moving. Plastic prisms, like the ones in prism bars or loose lens sets. should be held parallel to the face.
This is important because the effective deviation of the prism changes based on how you hold it in front of the eye; the BCSC gives an example of a glass prism that is held parallel to the face that has a reduced prismatic effect.
Glass prisms in a trial lens set.
Image credit: Bernell.com
Loose plastic prisms.
Image credit: eBay.
Plastic prism bars.
Image credit: Gulden Ophthalmics
Correct positions for holding glass and plastic prisms.
Illustration developed by Edmond H. Thall, M.D., and Kevin M. Miller, M.D., and rendered by C. H. Wooley.
Image credit: American Academy of Ophthalmology. Used with permission.
Real and Virtual Objects vs. Images
One of those pesky optics questions is talking about the differences between something real vs. virtual, and the differences between objects and images. With prisms, this is important for the sake of understanding how to use prisms to measure strabismus using various techniques.
I spent about 15 minutes reading and re-reading the 2 paragraphs in the BCSC discussing this concept, and basically came to the following conclusion:
When talking about real images (i.e., a projected light source or laser focused through a prism), the image is shifted toward the base. When talking about virtual images (i.e., our perception of an object through a prism lens), the image is shifted toward the apex.
In a patient with normal alignment (orthophoria), the patient will report seeing only one circle/light (red or white, depending on which eye is dominant).
Clinical Example
An example of this concept that I commonly use in my neuro-ophthalmology clinic is the the red glass test for measuring strabismus. In the red glass test, a red glass is placed over the right eye while the patient is looking at a white circle or light source. If the eyes are aligned or there is suppression, the patient will only see 1 circle/light (red or white). However, if there is some misalignment, the red glass dissociates the images (1 red circle/light and 1 white circle/light). To measure the misalignment, prisms are then placed in front of the right eye to "move" the circles/lights together.
I typically ask the patient, "where is the red circle/light compared to the white?" As long as the patient is able to accurately tell you if the red circle/light is to the right, left, above, or below the white circle/light, you can neutralize the deviation using loose prisms or a prism bar.
Example case: The red circle/light is to the right of the left circle/light (esotropia)
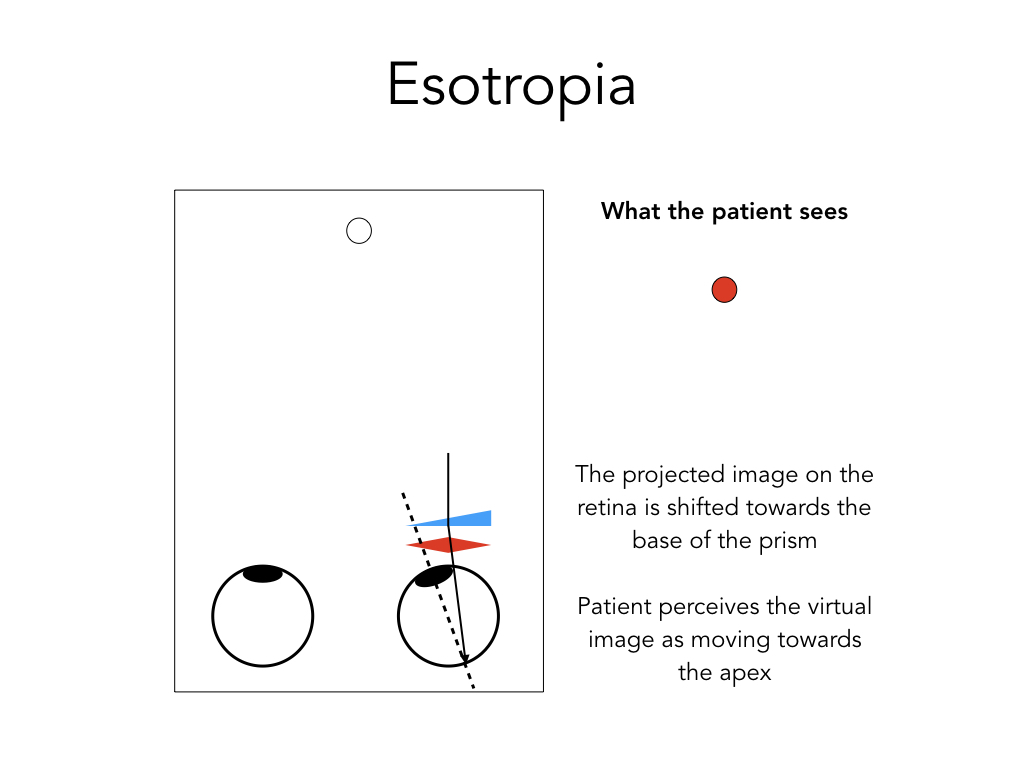
In esotropia, the image that is being projected onto the retina is a real image and, in the esotropic eye, will be focused nasal to the fovea (left figure). Because the area of the nasal retina corresponds to the temporal visual field, the perceived image (the virtual image) appears temporal to its real location.
By placing a base out prism in front of the eye (which is the treatment for esotropia), the real image is shifted towards the base of the prism and will focus on the fovea. This results in the merging of the two images. The patient would then, in essence, perceive the image moving towards the apex of the prism (or, the virtual image moves towards the apex of the prism).
I do want to note that when I am in clinic, I never think about this principle to this degree. I just point the apex of the prism in the direction I want the perceived image to go - in this example, because the red circle/light is to the right of the white, I point the apex to the left so that I "push" the perceived image to the left. This is essentially the same explanation as before, but intuitively it makes my prism measurements much faster.
Example Question
A patient presents with 20 Δ of exotropia and a fixation preference of the left eye. Where is the real image on the retina after the placement of a base-in, 10 Δ prism in front of the right eye?
A. Nasal to the optic nerve
B. Between the fovea and optic nerve
C. On the fovea
D. Temporal to the fovea
Answer: D. A patient with exotropia will have a real image projected temporal to the fovea. After placement of a base-in, 10 Δ prism over the right eye, the exotropia will be partially corrected but not completely corrected - as such, the real image will still be temporal to the fovea.
References and Additional Reading
- Basic and Clinical Science Course, Section 3. Clinical Optics. San Francisco: American Academy of Ophthalmology, 2017: 56-61.
- Wiggins MN, Pemberton JD. Clinical Optics Made Easy. Little Rock: Crimson House Publishing, 2018: 199-239.
Was this helpful? Did I get anything wrong? Do you have another way of thinking about prisms? Leave a comment or contact us!