Neuro-ophthalmology tends to have some of the more challenging questions, depending on your level of knowledge or comfort with these topics. One of the important things to recognize and evaluate is the swollen optic nerve.
Papilledema
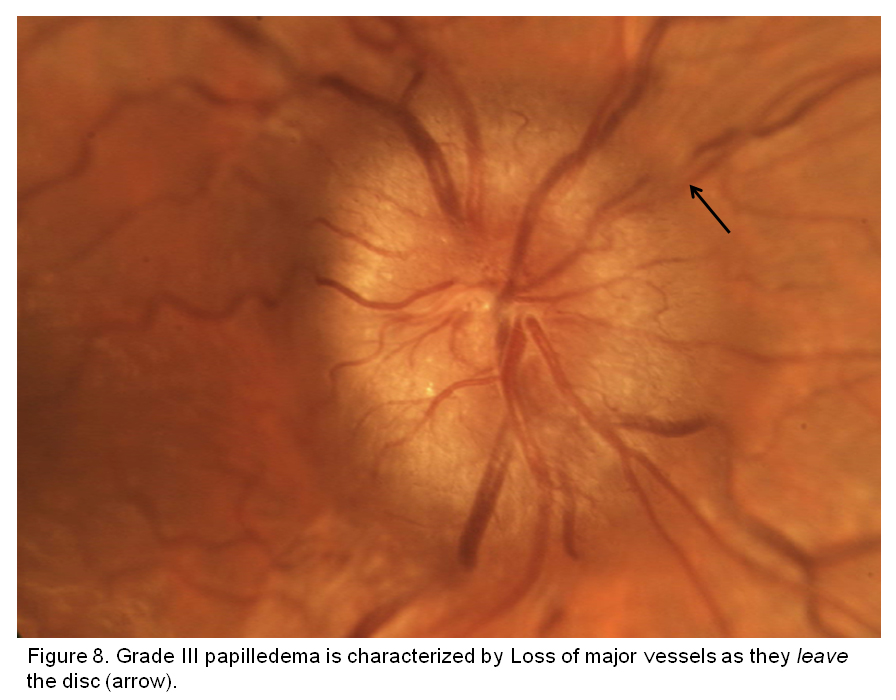
Image credit: University of Iowa.
Papilledema, strictly defined, refers to optic nerve swelling (typically bilateral - for the test think of it this way) associated with increased intracranial pressure.
Key Facts
- CSF is produced by the choroid plexus in the lateral ventricles, and absorbed by the arachnoid granulations in the venous sinuses.
- Causes include the following:
- Idiopathic intracranial hypertension (see below)
- Intracranial mass
- Hydrocephalus
- Craniosynostoses (especially Crouzon and Apert syndromes)
- Meningitis and other CNS infections
- Arteriovenous malformations
- Venous thromboses
- Inflammatory demyelinating polyneuropathies (AIDP and CIDP)
- POEMS syndrome (polyneuropathy, organomegaly, endocrinopathy, monoclonal gammopathy, and skin changes)
- Multiple myeloma
- Medications (see below)
- Symptoms of increased intracranial pressure include transient visual obscurations (blurred/decreased vision lasting seconds associated with bending over or Valsalva), headache, pulsatile tinnitus, and diplopia (which can be secondary to CN6 palsy, CN4 palsy, or skew deviation).
- An enlarged blind spot is the most common visual field defect.
- Over time visual fields will progress similar to glaucoma - nasal step, arcuate defects, tunneling, central scotoma.
- Normal intracranial pressure is around 8-20 cmH2O (21-25 cmH2O is borderline).
- Chronic papilledema will have optic nerve pallor, gliosis, optociliary (retinochoroidal) shunt vessels, and lipid refractile bodies.
Chronic papilledema. The optic nerves remain elevated with blurred margins, with feathering of the retinal nerve fiber layer. The nerve can become more atrophic and pale. Retinochoroidal (optociliary) shunt vessels can form due to the chronic outflow obstruction (black arrow in left image). Refractile bodies representing lipid exudates can also be seen (black arrow in right image).
Image credit: Acheson JF. Idiopathic intracranial hypertension and visual function. Br Med Bull. 2006;79-80:233-244.
Idiopathic Intracranial Hypertension
Idiopathic intracranial hypertension (pseudotumor cerebri) is the most common cause of papilledema. Here are a few basic facts:
- Classically, IIH affects young obese women ages 20-40.
- IIH is a diagnosis of exclusion. If there is a cause found for increased intracranial pressure, then it is no longer IIH.
- Mandatory testing includes MRI ± MRV brain with and without contrast; lumbar puncture with opening pressure; CSF cytology, protein, glucose, and cultures; and thorough history.
- IIH is associated with obstructive sleep apnea.
- IIH is initially treated with Diamox (acetazolamide) 500 mg BID, titrating up to maximally tolerated.
- Topamax (topiramate) and Lasix (furosemide) have also been used anecdotally.
- Remember that Diamox and Topamax are sulfa medications.
- Weight loss (6% of body weight) is also helpful.
- Steroids may be used to help protect the optic nerve in severe cases prior to surgical management.
- Surgically, optic nerve decompression and CSF diversion (lumboperitoneal or ventriculoperitoneal shunt) may be helpful for protecting vision.
Drug-Associated Intracranial Hypertension
There are several medications that have been implicated in increased intracranial pressure:
- Tetracyclines
- Vitamin A
- Cyclosporine
Those three treatments have been strongly reported as causes of increased intracranial pressure. There are other, less established medications that have also been reported: steroid withdrawal, Accutane, nalidixic acid derivatives (such as fluoroquinolones), and oral contraceptives.
Cerebral Venous Thrombosis
MRV demonstrating thrombosis of the right transverse and sigmoid sinuses (black arrows).
Image credit: Saposnik G, Barinagarrementeria F, Brown Jr. RD, et al. Diagnosis and Management of Cerebral Venous Thrombosis: A Statement for Healthcare Professionals From the American Heart Association/American Stroke Association. American Heart Association Stroke Council and the Council on Epidemiology and Prevention. Stroke. 2011;42:1158-1192.
- Cerebral venous thromboses most commonly involves the superior sagittal and transverse (lateral) sinuses.
- While an MRV is no longer required in typical presentations of papilledema, it should be ordered in atypical cases.
- If a CVT is found, anticoagulation and workup for hypercoagulable states should be initiated. On a practical level, this may warrant hospital admission or urgent referral to a neurologist.
Foster Kennedy Syndrome
Foster Kennedy Syndrome. It is classically described as ipsilateral optic atrophy with contralateral papilledema in the setting of a compressive optic neuropathy. In this case, the lesion would be compressing the left optic nerve.
Image credit: Pastora-Salvador N, Peralta-Calvo J. Foster Kennedy syndrome: papilledema in one eye with optic atrophy in the other eye. CMAJ. 2011;183:2135.
Foster Kennedy syndrome is a cause of contralateral papilledema as a result of compressive optic neuropathy. Associated with various frontal lobe, olfactory groove, and anterior clinoid tumors, there is typically ipsilateral optic atrophy with contralateral papilledema. Pseudo-Foster Kennedy syndrome is more common and typically represents acute NAION with contralateral optic atrophy from a previous NAION (see below).
POEMS Syndrome
An overview of the findings in POEMS syndrome.
Image credit: Dispenzieri A, Buadi FK. A review of POEMS syndrome. Oncology (Williston Park). 2013;27:1242-50.
POEMS is a rare paraneoplastic syndrome that has a ton of systemic manifestations, including increased intracranial pressure. While the likelihood of POEMS showing up on an OKAP or board exam is very low, I could also see a question like this popping up as one of the "separator"-type questions for those aiming for the top scores, which is why I include it here.
References and Additional Reading
- Basic and Clinical Science Course, Section 5: Neuro-Ophthalmology. American Academy of Ophthalmology, 2017-2018.
Is there anything else about papilledema that should be included in this review? Do you have any suggestions or requests for topics to cover? Leave a comment or contact us!