To be honest, I wasn't completely sure whether to categorize this topic under oculoplastics or ophthalmic pathology. Arguments definitely could be made for either, or both.
In any case, there are 3 major tumors that affect the lacrimal gland: orbital lymphoma, pleomorphic adenoma of the lacrimal gland, and adenoid cystic carcinoma of the lacrimal gland. If you see a test question about a tumor of the lacrimal gland, it is going to be one of those three conditions (probably).
Lacrimal Gland Histology (A Brief Review)
Normal lacrimal gland histology.
Image credit: Mission For Vision.
Lacrimal gland tissue is unique to ophthalmology in that, of all the different histologic tissues we need to know for the OKAP (and other exams), the lacrimal tissue is the only acinar gland. There are accessory lacrimal glands that also contribute to the aqueous tear layer, but, as an ophthalmic pathologist once said at a review conference I attended, "if you see this tissue, think lacrimal gland."
Orbital Lymphoma
External exam of orbital lymphoma. Note the "salmon patch" appearance of the conjunctiva, which is a key clinical descriptor of orbital lymphoproliferative conditions.
Image credit: khanfacial.com
Key Facts
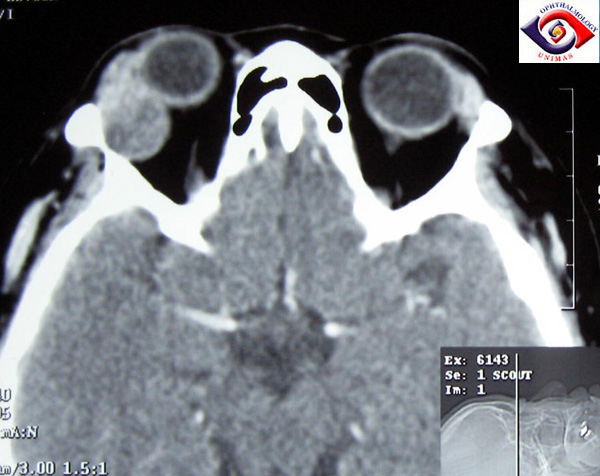
CT coronal scan showing the putty-like molding of orbital lymphoma to ocular structures.
Image credit: sarawakeyecare.com.
- Orbital lymphoma comprises over 20% of all lacrimal tumors.
- Most cases of orbital lymphoma are of B-cell origin.
- They typically present slowly, progressively, and painlessly. Most cases are unilateral. They will often cause proptosis or mass shift of the globe as it grows.
- 50% of orbital lymphomas arise from the lacrimal fossa.
- If there is a conjunctival component, or if the lesion extends onto the globe, it can be seen as a salmon-patch lesion on or under the conjunctiva (as shown above).
- Radiographically, orbital lymphoma differs from other lacrimal gland tumors in that it has a "putty-like" molding to the orbital structures (because it is not an encapsulated tumor or mass, the lymphoma cells migrate along the surface of everything it touches).
- Orbital lymphoma can be seen in both CT and MRI.
- Most lymphomas around the eye arise from mucosa-associated lymphatic tissue (MALT).
- MALT lymphomas are associated with chronic Chlamydial (found by PCR in 80% of conjunctival MALT lymphomas) and H. pylori infections, although MALT lymphomas associated with H. pylori infection are more often present in the GI tract.
- 50% of MALT lymphomas will develop systemic disease at 10 years!
- Treatment is typically low-dose orbital radiation, with chlorambucil and doxycycline (100 mg BID x 3 weeks) having some beneficial effects as well.
Histopathology
Histopathology of MALT lymphoma. Note the relatively uniform appearance of the blue cells.
Image credit: Mission For Vision.
Lymphomas are characteristically described as "sheets of blue cells." There are very few stromal components, but rather a homogeneous mass of atypical lymphocytes. Unlike most lymphoid tissue (and benign lymphoproliferation), lymphomas have poorly-defined follicles.
- Diagnosis is typically achieved by a combination of history, examination, diagnostic imaging, and biopsy.
- If lymphoma is suspected, an incisional biopsy with fresh, unfixed tissue is submitted for cell surface markers and flow cytometry.
- Because fresh tissue has to be submitted, careful coordination should be taken with the pathologist to ensure proper handling of the tissue.
- On immunohistochemistry staining, these lymphomas are typically monoclonal, and will typically stain for B cells (CD19 and CD20).
Pleomorphic Adenoma (Benign Mixed Tumor)
Key Facts
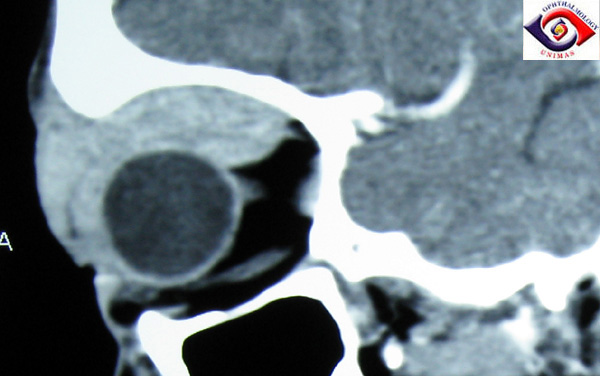
CT axial image of a large lacrimal gland mass. It is well-encapsulated, reflecting the pseudoencapsulation of the tumor.
Image credit: sarawakeyecare.com.
- Pleomorphic adenomas are the most common lacrimal gland epithelial tumor. It accounts for 50% of all lacrimal gland epithelial tumors.
- They typically present in young adults (age 30-50), and affect men more than women.
- They are slowly progressive (as in may take years to grow), and are painless.
- They are pseudoencapsulated.
- Globe displacement is typically down/in or axial.
- Pleomorphic adenomas do not invade the bone - they may erode the bone and induce reactive bone formation in a process called cortication.
- While pleomorphic adenomas are typically benign, long-standing tumors (>15 years) may degenerate into malignant lesions such as adenoid cystic carcinoma, malignant mixed tumor, or adenocarcinoma.1
- Treatment is complete excisional biopsy with preservation of pseudocapsule.
- Partial excision has a high recurrence rate (32%). This is bad, because recurrences are associated with a malignant transformation rate of 10% per 10 years.
Histopathology
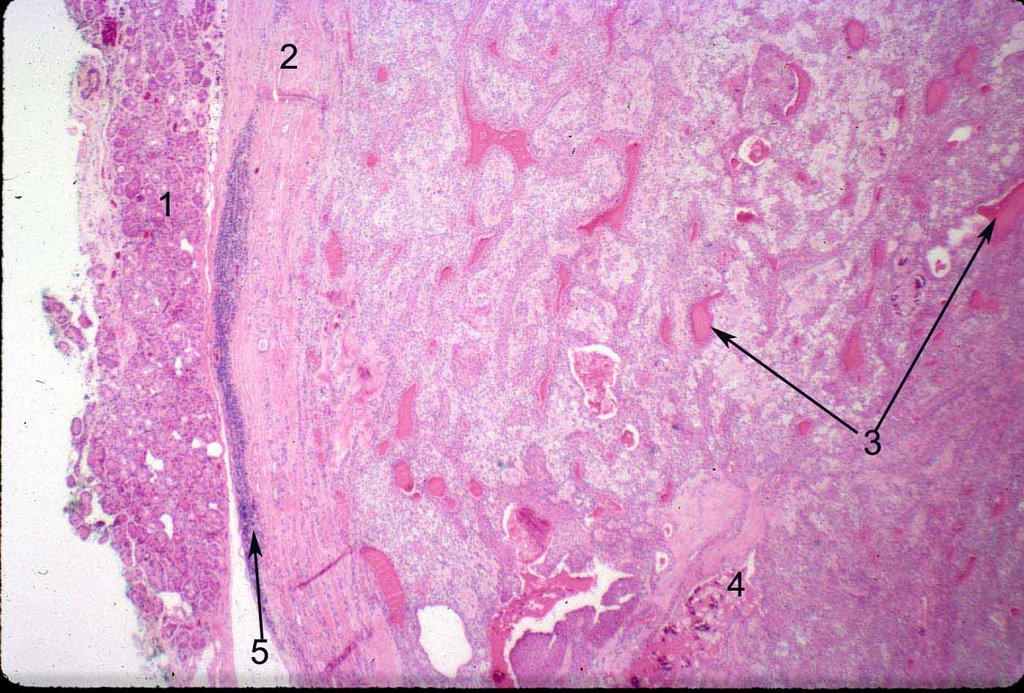
Histopathology of a pleomorphic adenoma. The pseudocapsule is featured on the left (2), pushing the normal lacrimal gland tissue aside (1). Epithelial ducts (3) and calcification may be present (4), and chronic inflammation may be present along the edge of the pseudocapsule (5).
Image credit: Mission For Vision.
Histopathology of pleomorphic adenoma. There are stromal elements (6) and epithelial hyaline/basement membrane material (7) present, as well as seromucinous material (8).
Image credit: Mission For Vision.
Histopathology of pleomorphic adenoma. There can be cartilaginous material (8) present, as well as hyaline/basement membrane material (9). Epithelial cells form cords and ducts (10).
Image credit: Mission For Vision.
- Pleomorphic adenomas may also be called benign mixed tumors because they contain both epithelial and stromal components.
- They are one of two orbital tumors that contain cartilage. Teratomas are the other orbital tumor containing cartilage.
- On immunohistochemistry, pleomorphic adenomas stain positive for epithelium (keratin, epithelial membrane antigen) & myoepithelium (keratin, actin, myosin, fibronectin, S-100).
Adenoid Cystic Carcinoma (Cylindroma)
Key Facts
- Adenoid cystic carcinoma is the most common malignant lacrimal gland tumor. It accounts for 25% of all epithelial lacrimal gland tumors.
- It arises de novo or from a recurrent pleomorphic adenoma.
- It typically presents in adults between 30-50 years old; the median age is 40 years old.
- It affects women more than men, which is opposite of pleomorphic adenoma.
- They are rapidly growing (enlargement takes place on the scale of months), and are painful.
- They are infiltrative in nature, lacking encapsulation, and will erode bone.
- They invade nerves (perineural invasion), causing severe pain.
- The event that initiates the formation of adenoid cystic carcinoma is the loss of the 1p36 gene.
- Treatment is usually quite drastic - exenteration, radical orbitectomy, bone removal, and radiation with debulking. Unfortunately, these treatments do not improve survival rates.
- Recurrences are usually multiple and painful.
- In most of these patients, intracranial extension is fatal after at least 10 years.
- Genetic testing of the tumor can be helpful:
- bcl-2 and bax expression carries a good prognosis.
- p53 expression carries a worse prognosis.
Histopathology
Histopathology of adenoid cystic carcinoma. The characteristic description is the "swiss cheese" (cribriform) appearance, which is actually formed by back-to-back ducts with no intervening stroma (1). This is most common form, though there are other forms as well.
Image credit: Mission For Vision.
Histopathology of adenoid cystic carcinoma. This part of the tumor has far fewer ducts and is represented mostly by solid sheets of blue cells (basaloid cells), especially in the top portion of the image. This is characteristic of the basaloid variant, which carries a much worse prognosis.
Image credit: Mission For Vision.
Histopathology of adenoid cystic carcinoma, basaloid type. This slide demonstrates perineural invasion. The blue basaloid cancer cells (3) have surrounded the normal nerve tissue (2).
Image credit: Mission For Vision.
Histopathology of adenoid cystic carcinoma, cribriform type. This is another example of perineural invasion, but with the ductal cells (3) surrounding normal nerve tissue (4) rather than the blue basaloid cells.
Image credit: Mission For Vision.
Histopathology of adenoid cystic carcinoma, basaloid type. This slide points out a mitotic figure (5), which suggests aggressive cancerous activity.
Image credit: Mission For Vision.
- Adenoid cystic carcinoma can appear histologically in several different patterns.
- The most common type of adenoid cystic carcinoma is the cribriform, or "Swiss cheese" pattern, shown in the first figure.
- The other type you may need to recognize is the basaloid type, in which the tumor grows in a solid nest of blue cells. The basaloid type carries the worst prognosis (20% 5-year survival rate, vs. 70% 5-year survival rate for non-basaloid types).
- Other types include the comedo, sclerosing, and tubular patterns (probably not as important to recognize).
- Immunohistopathology staining is the same as pleomorphic adenoma, staining positive for epithelium (keratin, epithelial membrane antigen) & myoepithelium (keratin, actin, myosin, fibronectin, S-100).
Key Distinctions In Lacrimal Gland Lesions
References and Additional Reading
- What Is Pleomorphic Adenoma? Mission For Vision. Website. Accessed February 2, 2016.
- MALT Lymphoma. Mission For Vision. Website. Accessed February 2, 2016.
- What Is Adenoid Cystic Carcinoma Of Lacrimal Gland? Mission For Vision. Website. Accessed February 2, 2016.
- Basic and Clinical Science Course, Section 4: Ophthalmic Pathology and Intraocular Tumors. American Academy of Ophthalmology, 2017-2018.
- Basic and Clinical Science Course, Section 7: Orbit, Eyelids, and Lacrimal System. American Academy of Ophthalmology, 2017-2018.
Is there anything else about lacrimal gland tumors that you think is important? Do you have any suggestions or requests for review topics? Leave us a comment or contact us!