Papilledema with pseudopapilledema features.
Papilledema is optic nerve edema secondary to increased intracranial pressure. The optic nerves are hyperemic, with whitish opacification of the peripapillary retinal nerve fiber layer. Telangiectatic vessels are seen on the temporal optic disc in the left eye. In severe cases of papilledema the retinal vasculature will become obscured by the nerve fiber layer edema.
In this case, the appearance of the optic nerve is confounded by yellowish refractile bodies on the nasal aspect of both optic nerves and the anomalous branching appearance of the retinal vessels in the left optic nerve. There is some nerve fiber layer whitening most pronounced in the superior aspect of the right optic nerve, and the retinal vessels are not obscured.
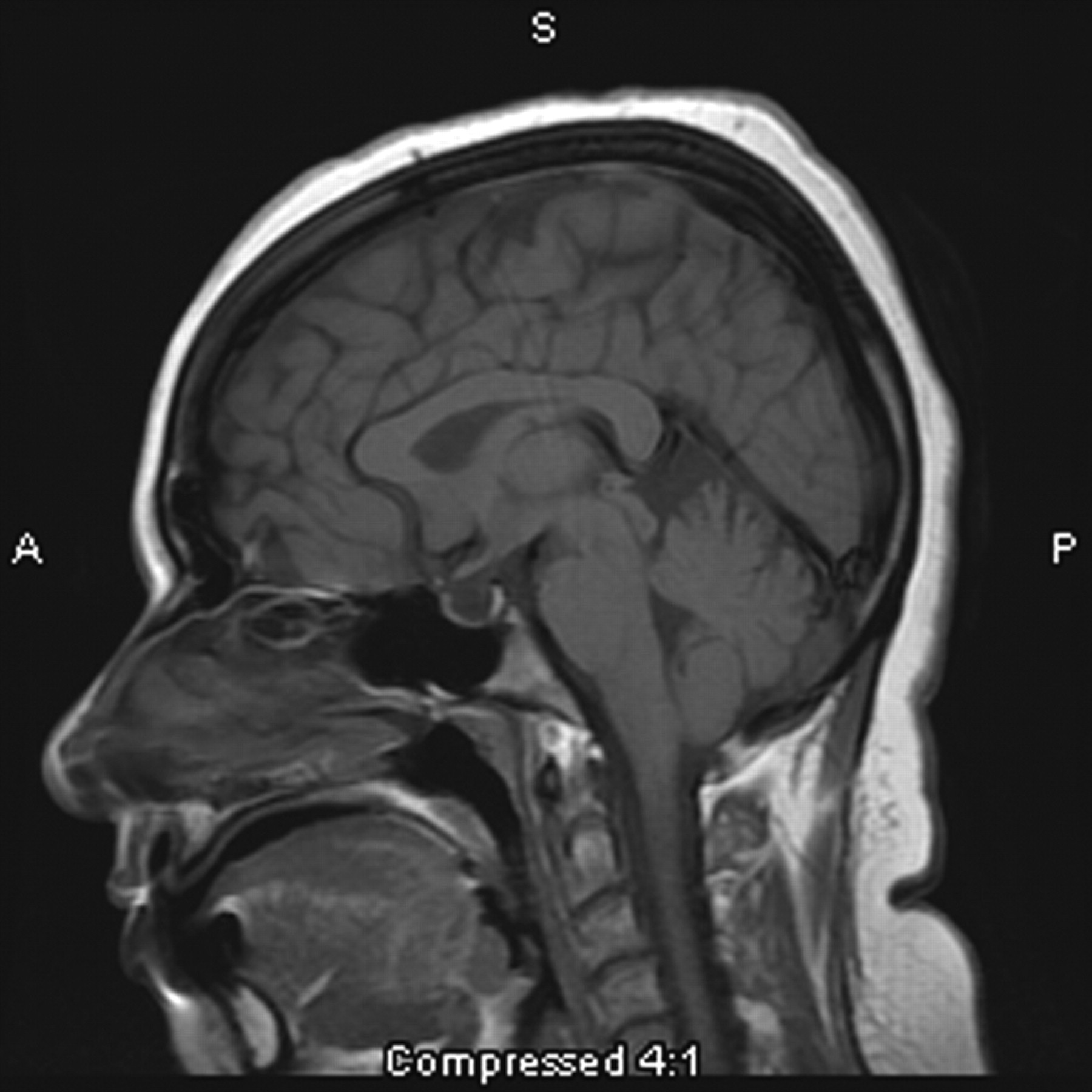
Differentiating papilledema from pseudopapilledema is extremely difficult based on clinical appearance alone. The presence of pseudopapilledema does not exclude papilledema. Ancillary testing that may help differentiate between papilledema and pseudopapilledema include OCT, autofluorescence, fluorescein angiography, and ultrasound. In cases where the diagnosis remains in doubt clinically, the patient should be counseled regarding whether to proceed with further workup for intracranial hypertension (MRI/MRV brain, LP with opening pressure, CSF studies) or to observe. This is often guided by the patient’s symptoms and the clinical suspicion for increased intracranial pressure.
Image credit: American Academy of Ophthalmology. Used with permission for educational purposes.