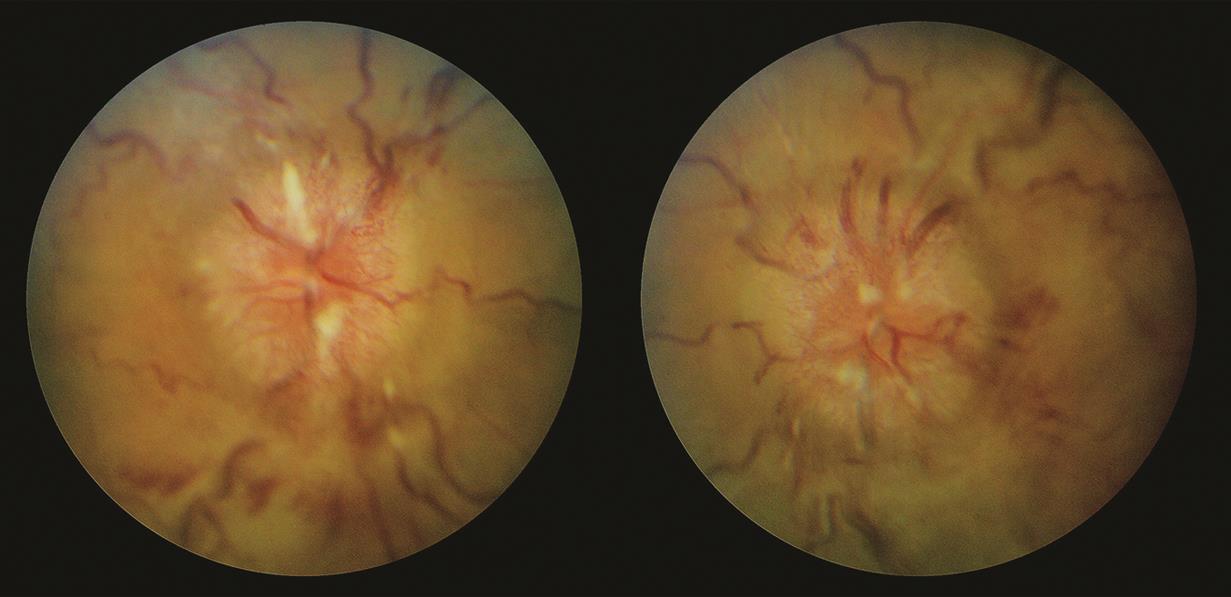
Chronic papilledema from superior sagittal sinus thrombosis.
In the right eye, the optic nerve is diffusely elevated with nerve fiber layer edema. There is some mild tortuosity to the retinal vessels, and the smaller retinal vessels are obscured at the margins of the optic nerve. This is characteristic of Frisén grade 3 papilledema. Just temporal to the optic nerve are very faint dark lines concentric to the optic nerve. These are retinal folds (Paton lines), which can be seen in papilledema.
In the left eye, the optic nerve is diffusely elevated with nerve fiber layer edema. There is also some mild tortuosity, but the retinal vessels do not appear obscured by the nerve fiber layer edema. This is characteristic of Frisén grade 2 papilledema.
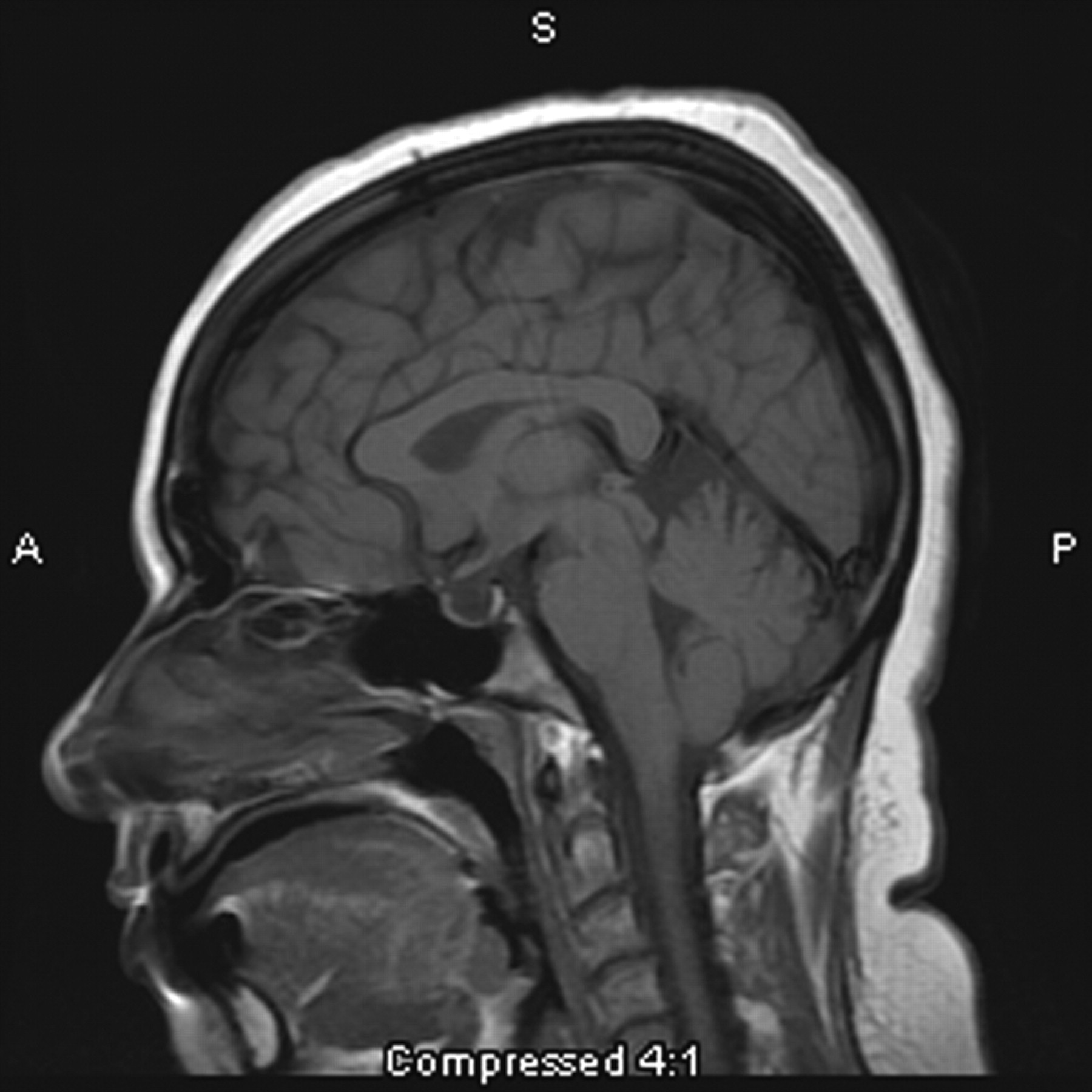
Because idiopathic intracranial hypertension is a diagnosis of exclusion, all patients with suspected papilledema need to be worked up for secondary causes of intracranial hypertension with an MRI ± MRV brain, lumbar puncture with opening pressure, and cerebrospinal fluid (CSF) studies.
Image credit: Schiefer, Wilhelm, Hart (Eds.). Clinical Neuro-Ophthalmology - A Practical Guide. Springer: Berlin/Heidelberg/New York, 2007. Used for educational purposes.