Video credit: Lee AG. NAION. Video. YouTube. Available online. Accessed 2 July 2019.
Non-Arteritic Anterior Ischemic Optic Neuropathy
Optic atrophy following non-arteritic anterior ischemic optic neuropathy, right eye.
Left: Patient’s right eye. Note the pale color of the superior aspect of the optic nerve with loss of the peripapillary capillary network.
Right: Patient’s left eye. The optic nerve is crowded (no discernable cup-to-disc ratio). The optic nerve color is generally normal.
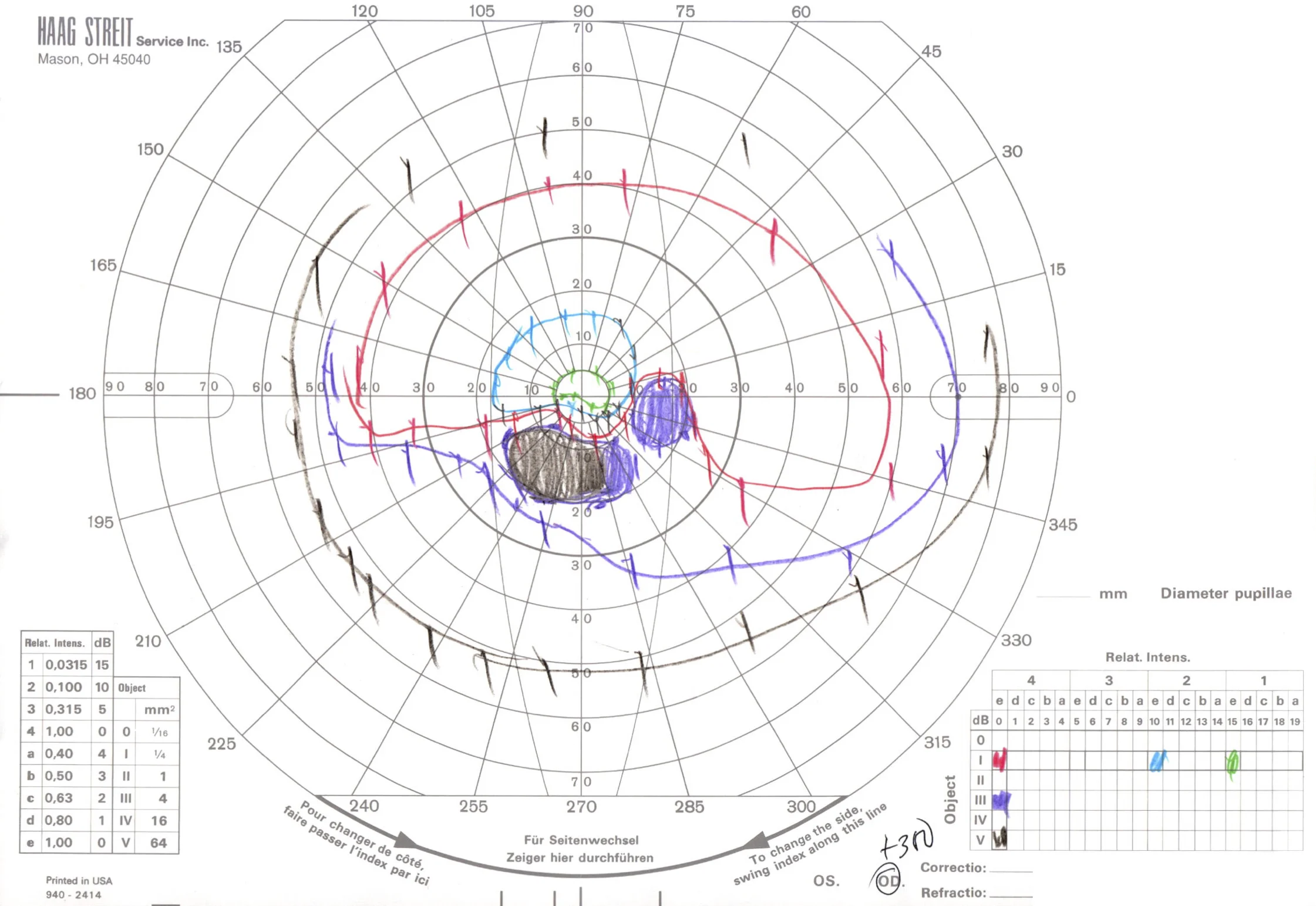
Goldmann (top) and automated (bottom) perimetry of the same patient demonstrating an incomplete inferior altitudinal visual field defect in the right eye and a mild inferotemporal visual field defect in the left eye. Although the left optic nerve appeared grossly normal, it was hypothesized that the left optic nerve may have suffered a mild injury, resulting in the reproducible visual field defect.
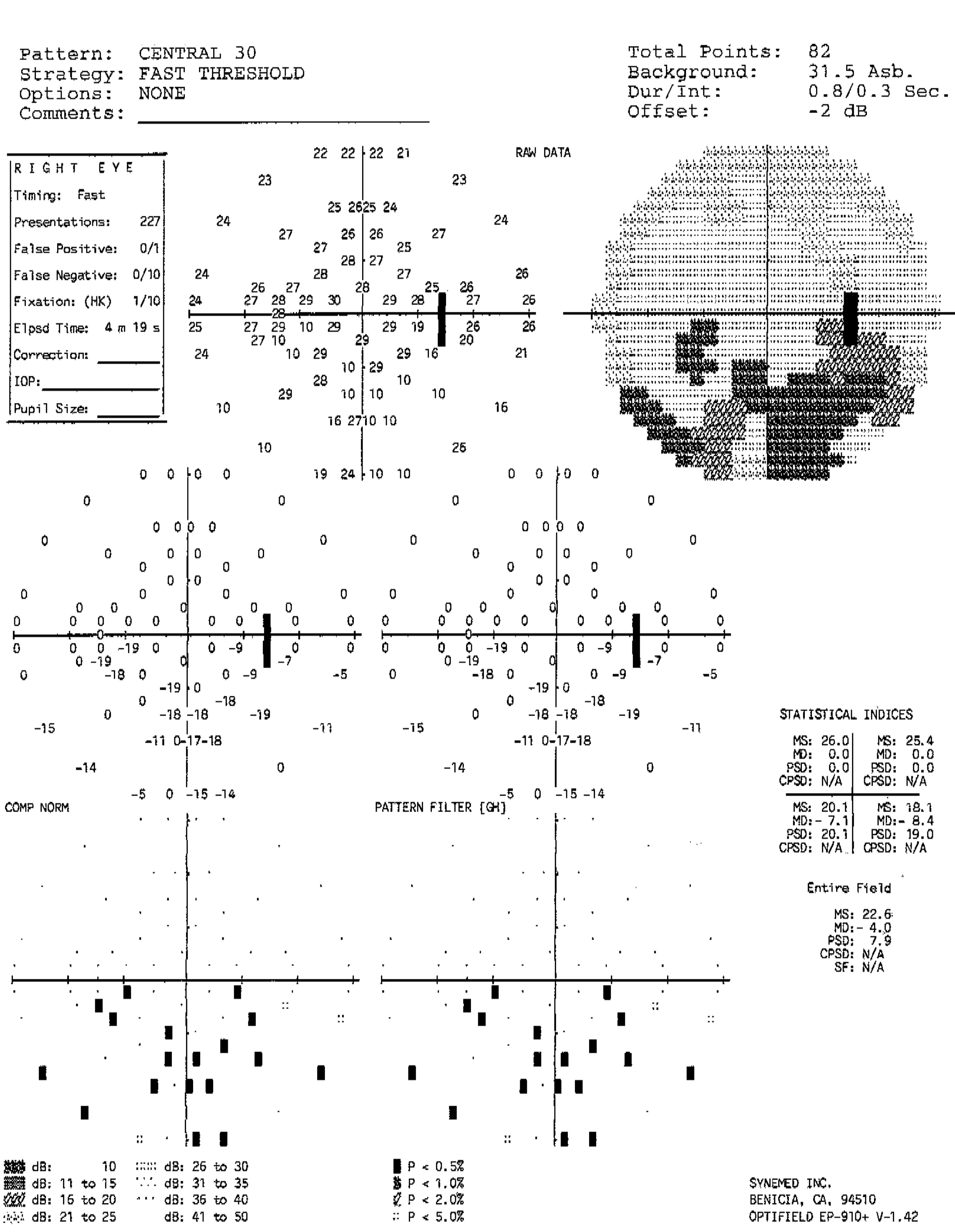
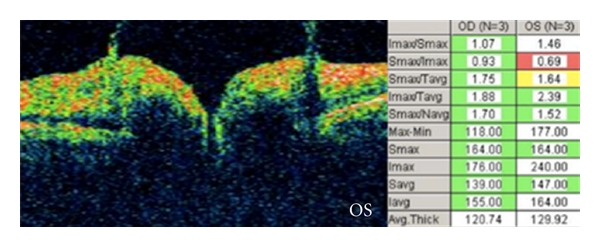
Optical coherence tomography of the macula demonstrating an essentially normal fovea in each eye. This patient presented with optic atrophy, but with a history of optic nerve edema noted by an outside ophthalmologist. Because a branch retinal artery occlusion can also result in similar visual field defects and sectoral optic atrophy, an OCT of the macula helped confirm the preservation of the inner retina, which supports the diagnosis of NAION.
Optical coherence tomography of the macula showing loss of the inner retina in branch retinal artery occlusion (different patient, left eye). In contrast to the previous OCT, there is a complete loss of the foveal contour and the inner layers of the retina are thinned and less defined than the normal right eye.
Non-Arteritic Anterior Ischemic Optic Neuropathy
Non-arteritic anterior ischemic optic neuropathy (NAION).
Note the hyperemia of the optic nerve and nasal edema. The nerve fiber layer edema obscures retinal vessels (most noticeable superiorly). The optic nerve is small and crowded. There are also flame/splinter/nerve fiber layer hemorrhages.
Image credit: American Academy of Ophthalmology. Used with permission for educational purposes.
Anterior Ischemic Optic Neuropathy
Anterior ischemic optic neuropathy (AION).
Diffuse optic nerve edema with flame/splinter/nerve fiber layer hemorrhages, telangiectasias, and nerve fiber layer whitening.
By definition, anterior ischemic optic neuropathy necessitates the presence of optic nerve edema, either by history (noted by other physicians), fundus photography, or other objective methods. AION never presents acutely with a normal or pale optic nerve.
Image credit: American Academy of Ophthalmology. Used with permission for educational purposes.
Non-Arteritic Anterior Ischemic Optic Neuropathy and Arteritic Anterior Ischemic Optic Neuropathy
Non-arteritic anterior ischemic optic neuropathy vs. arteritic anterior ischemic optic neuropathy.
ONH appearance in nonarteritic anterior ischemic optic neuropathy (NAION) and arteritic anterior ischemic optic neuropathy (AAION).
A) The healthy eye demonstrates a characteristic crowded appearance, which has been called “disc at risk.”
B) ONH appearance in NAION. Edema is segmental, with mild superimposed pallor and flame hemorrhages.
C) The healthy eye demonstrates a normal cup–disc ratio. Lack of a disc at risk should suggest an AAION.
D) ONH appearance in AAION. Pallor is more pronounced.
Image credit: Parts A, B courtesy of Michael S. Lee, M.D.; parts C, D courtesy of Rod Foroozan, M.D.. American Academy of Ophthalmology. Used with permission for educational purposes.
Non-Arteritic Anterior Ischemic Optic Neuropathy
Non-arteritic anterior ischemic optic neuropathy, right eye.
a) Acute phase showing hyperemia, superior optic nerve edema with telangiectatic vessels, and nasal nerve fiber layer (flame/splinter) hemorrhage.
b) Late phase showing segmental pallor superiorly. Note the healthy optic nerve tissue inferiorly and the preservation of the crowded cup-to-disc ratio.
Image credit: American Academy of Ophthalmology. Used with permission for educational purposes.
Vitreopapillary Traction
Vitreopapillary traction. Note the mild peripheral obscuration of retinal vessels in both eyes with relative preservation of the optic disc margins.
Optical coherence tomography of vitreopapillary traction (same patient). Bilateral vitreopapillary traction noted.
Fluorescein angiography of vitreopapillary traction (same patient). Note the mild focal leakage seen in both eyes (perhaps slightly more prominent in the left eye).
Image credit: Houle E, Miller NR. Bilateral vitreopapillary traction demonstrated by optical coherence tomography mistaken for papilledema. Case Rep Ophthalmol Med 2012;2012:682659. doi: 10.1155/2012/682659. Available online. Used for educational purposes.
Vitreopapillary Traction
Vitreopapillary traction. A, Photograph of the right optic nerve shows disc elevation, blurred margins, and obscuration of nasal vessels. B, Transverse optical coherence tomography reveals peripapillary vitreous adhesion and traction, resulting in elevation of the optic disc and peripapillary retina.
Image credit: Simonett JM, Winges KM. Vitreopapillary traction detected by optical coherence tomography. JAMA Ophthalmol 2018;136(5):e180727. doi: 10.1001/jamaophthalmol.2018.0727. Available online. Used for educational purposes.
Vitreopapillary Traction
Vitreopapillary traction. The condensation of vitreous over the optic nerve can cause the optic nerve to look blurred, and the traction itself can result in elevation of the optic nerve and blur the edges of the optic nerve.
Image credit: Courtesy of Alex P. Hunyor, M.D. Retina Image Bank. American Society of Retina Specialists. Available online. Used for educational purposes.
Prepapillary Hemorrhage
Prepapillary hemorrhage. Partial posterior vitreous detachment in a myopic Asian patient.
Image credit: Katz B, Hoyt WF. Intrapapillary and peripapillary hemorrhage in young patients with incomplete posterior vitreous detachment. Signs of vitreopapillary traction. Ophthalmology 1995;102(2):349-54. Spencer S. Eccles Health Sciences Library, University of Utah, 2002. Neuro-ophthalmology Virtual Education Library. Available online. Used for educational purposes.
Glial Veil
Glial veil.
Image credit: American Academy of Ophthalmology. Used with permission for educational use.
Glial Tuft
Glial tuft.
Image credit: American Academy of Ophthalmology. Used with permission for educational purposes.
Bergmeister Papilla
Bergmeister papilla (histopathology). A, Gross photograph of infant eye showing fingerlike projection of whitish tissue (arrow) from the surface of the optic nerve head. B, Low-magnification photomicrograph of part A showing fibroglial tissue (arrow) projecting into the vitreous cavity from the optic nerve head. C, High-magnification photomicrograph of Bergmeister papilla demonstrating loose fibrous connective tissue with small capillary (arrow), surrounded by a thin layer of fibrous astrocyte-like cells (arrowhead).
Image credit: Courtesy of Robert H. Rosa, Jr., M.D. American Academy of Ophthalmology. Used with permission for educational purposes.
Bergmeister Papilla
Bergmeister papilla.
Image credit: Courtesy of Kathleen Digre, M.D. Spencer S. Eccles Health Sciences Library, University of Utah, 2012. Neuro-ophthalmology Virtual Education Library. Available online. Used for educational purposes.
Crowded Optic Nerve
Crowded optic nerves. Note the anomalous vasculature and scalloped edges of the optic disc.
Image credit: Courtesy of William F. Hoyt, M.D. Spencer S. Eccles Health Sciences Library, University of Utah, 2002. Neuro-ophthalmology Virtual Education Library. Available online. Used for educational purposes.
Crowded Optic Nerve
Crowded optic nerve with glial remnant. Note the glial remnant in the right eye.
Image credit: Courtesy of William F. Hoyt, M.D. Spencer S. Eccles Health Sciences Library, University of Utah, 2002. Neuro-ophthalmology Virtual Education Library. Available online. Used for educational purposes.
Crowded Optic Nerve
Crowded congenital blurred disc. Note the anomalous vascular pattern and glial tissue on the disc in the right eye.
Image credit: Courtesy of William F. Hoyt, M.D. Spencer S. Eccles Health Sciences Library, University of Utah, 2002. Neuro-ophthalmology Virtual Education Library. Available online. Used for educational purposes.
Hyperopic Optic Nerve
Hyperopic optic nerve. Note the crowded appearance of the optic nerve with nasal elevation. There is mild venous tortuosity, which can suggest venous outflow congestion and obscure the diagnosis. There is some anomalous branching of the retinal vessels, suggestive of pseudopapilledema. Despite the elevation and crowding of the optic disc, there is no whitening of the peripapillary retinal nerve fiber, no obscuration of the retinal vessels, no retinal or choroidal folds, and no nerve fiber layer hemorrhages.
Image credit: Karl Golnik, M.D. on UpToDate. Available online. Used for educational purposes.
Hyperopic Optic Nerve
Hyperopic optic nerve. Note the generally ill-defined appearance to the optic nerve, with obscuration of the nasal contour. There is a small cup, and there may be a very slight elevation to the superior edge of the optic nerve. However, there is no whitening of the peripapillary nerve fiber layer, no obscuration of the retinal vessels, no venous engorgement or tortuosity, no true blurring of the nerve margins, no hemorrhages, and no retinal or choroidal folds.
Image credit: Appearance of optic nerve disorders. Entokey. Available online. Used for educational purposes.
Myelinated Nerve Fibers
Myelinated nerve fibers.
Image credit: Courtesy of Anthony C. Arnold, M.D. American Academy of Ophthalmology. Used with permission for educational purposes.