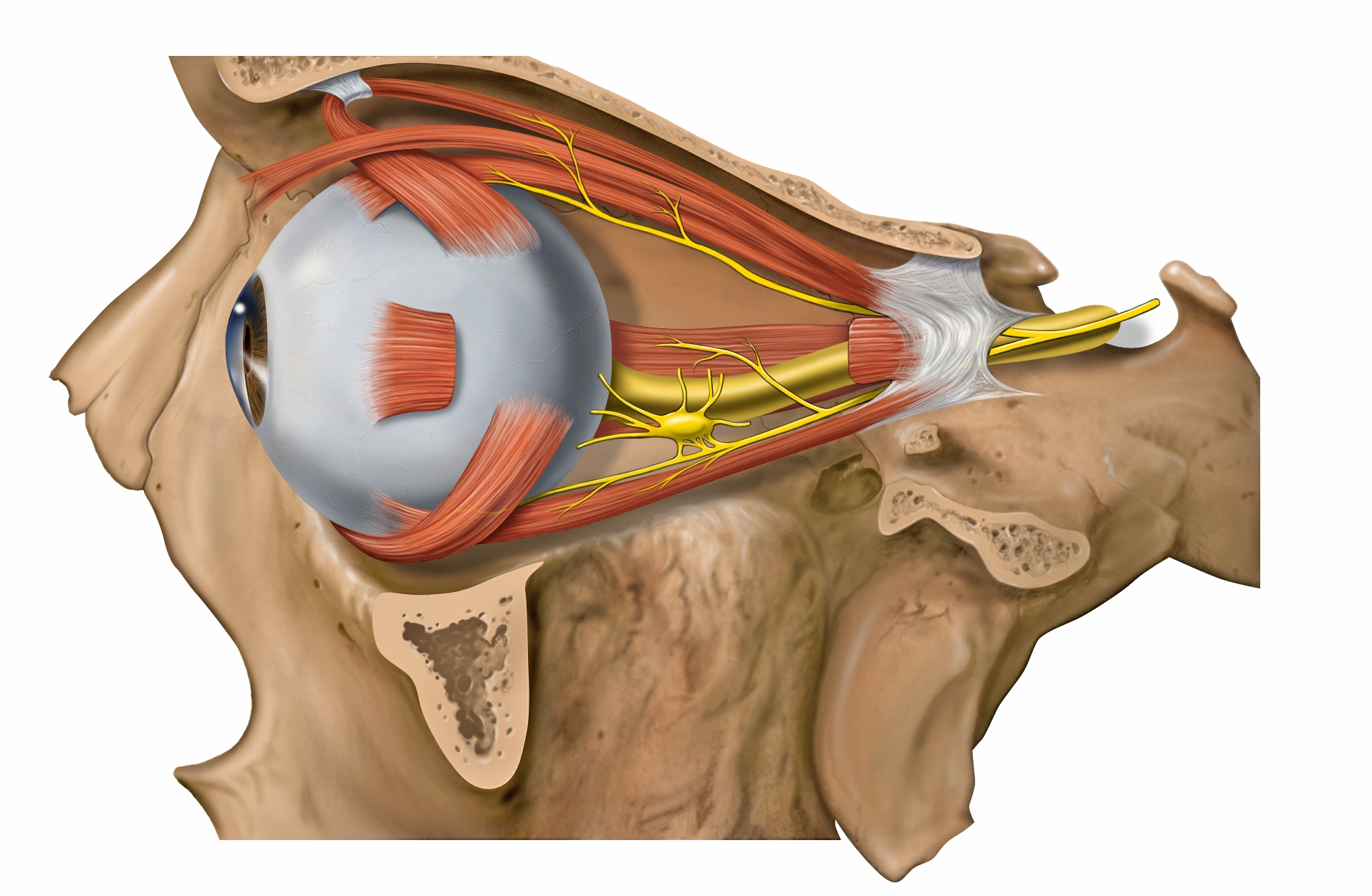
The ciliary ganglion lies temporal to the ophthalmic artery, inbetween the lateral rectus and optic nerve. It is approximately 1.5-2.0 cm (15-20 mm) posterior to the globe and 1.0 cm (10 mm) anterior to the Annulus of Zinn and the superior orbital fissure.
Image credit: Wikipedia.
The ciliary ganglion serves as the site of synapse for the parasympathetic nerves innervating the eye. Because of the many nerves that course through it (not all of them synapse!) and its anatomical location, this structure is of importance in learning the basics of ophthalmology. According to the Basic and Clinical Science Course, it is located lateral to the ophthalmic artery, situated between optic nerve and lateral rectus muscle, approximately 1 cm (10 mm) anterior to the annulus of Zinn and 1.5-2 cm (15-20 mm) posterior to the globe (1-5).
The ciliary ganglion is small, usually measuring 2 mm horizontally and 1 mm vertically. It receives its blood supply from the posterior lateral ciliary artery (supplying the anterior half of the ganglion) and from the lateral muscular arterial trunk (entering the ganglion from its lateral side) (2, 5).
Afferent Nerves
The sensory nerves that travel from the eye are actually fibers of the nasociliary nerve, a branch of the trigeminal nerve (V1). These fibers travel along the short and long ciliary nerves through the ciliary ganglion without synapsing and forms a sensory root exiting the ciliary ganglion posteriorly before merging with the nasociliary nerve, which course along V1 and ultimately synapse at the trigeminal ganglion (1).
For more information about the sensory nerves to the eye, stay tuned - this will be a separate article.
Efferent Nerves
Parasympathetic Nerves
Preganglionic (presynaptic) parasympathetic nerves arising from the Edinger-Westphal nucleus in the CN3 complex synapse in the ciliary ganglion. As you might guess, the parasympathetic fibers here mediate the pupil constriction (light) and accommodative responses. These fibers course along CN3, follow along the inferior division of CN3 when it splits at the level of the annulus of Zinn, and forms the motor root entering the ciliary ganglion, where they synapse.
The postganglionic (postsynaptic) parasympathetic nerves are myelinated. They course along the short ciliary nerves to innervate the iris sphincter (only 3-5% of the postganglionic parasympathetic fibers are pupillomotor!) and ciliary muscles (6-7).
Sympathetic Nerves
There are also postganglionic sympathetic fibers that course through the ciliary ganglion. These are NOT myelinated, and arise from the superior cervical ganglion, which is located near the angle of the jaw and the bifurcation of the common carotid artery. These sympathetic fibers do NOT synapse in the ciliary ganglion, and follow the long posterior ciliary nerves and short ciliary nerves to innervate the pupillary dilator muscle (1-2, 6)
Tips and Hints
- There are essentially 3 groups of nerves that course through the ciliary ganglion (sensory, parasympathetic, sympathetic).
- Only 1 group of nerves synapses in the ganglion (parasympathetic).
- The postganglionic parasympathetic nerves have a short distance to go to the eye and travel along the short ciliary nerves.
- The postganglionic sympathetic nerves travel a long distance from the superior cervical ganglion to get to the eye and travel along the long ciliary nerves. Keep in mind that some of the sympathetic nerves will also travel along the short ciliary nerves.
- The sensory nerves travel along both short and long ciliary nerves. They eventually merge with the nasociliary nerve (V1), which travels through the annulus of Zinn.
Clinical Correlations
Adie's Tonic Pupil and Holmes-Adie Syndrome
For more information about Adie's pupil, stay tuned - I plan to write a separate article (or more) about the subject.
Adie's tonic pupil is characterized by an idiopathic, sudden-onset denervation of the ciliary body and iris sphincter, followed by a slow abnormal reinnervation. This results in a sudden fixed, dilated pupil and loss of accommodation in that eye. Adie's tonic pupil is typically initially unilateral (80%), with increased risk of involvement of the contralateral pupil over time. The denervation occurs at the level of the ciliary ganglion, with aberrant regeneration of accommodation occurring over the course of the next 1-2 years. Other clinical features include segmental iris sphincter palsy, light-near dissociation, and cholinergic hypersensitivity. When in association with a loss of deep tendon reflexes (hyporeflexia or areflexia), it is called Holmes-Adie syndrome (8).
Ciliary Ganglion Injury
The ciliary ganglion can be injured directly or iatrogenically. Ocular and orbital surgeries that have been associated with ciliary ganglion injury include the following (8):
- Retinal attachment surgery (9)
- Inferior oblique muscle surgery (10)
- Orbital surgery (11)
- Optic nerve sheath fenestration (especially lateral orbitotomy approach) (12)
- Retinal photocoagulation (13-14)
- Argon laser trabeculoplasty (15)
- Transconjunctival cryotherapy
- Transscleral diathermy
- Retrobulbar alcohol
- Inferior dental blocks (16)
Ciliary Ganglion Injury Associated With Systemic Illness
There are some systemic infections and inflammations that have been reported to cause a tonic pupil, which includes the following (8):
- Herpes zoster (17)
- Chickenpox (18)
- Measles
- Diphtheria
- Syphilis (congenital and acquired) (8, 19)
- Lyme disease
- Sarcoidosis (20)
- Scarlet fever
- Pertussis
- Smallpox
- Influenza
- Sinusitis
- Vogt-Koyanagi-Harada syndrome (21)
- Rheumatoid arthritis (22)
- Polyarteritis nodosa (23)
- Giant cell arteritis (24-25)
- Migraine (26)
- Lymphomatoid granulomatosis (27)
- Viral hepatitis
- Choroiditis
- Primary and metastatic choroidal and orbital tumors (28)
- Blunt injury to the globe
- Intraocular siderosis (29)
- Penetrating orbital injury
Video Lecture
For those who want to listen to a 30-minute lecture on the ciliary ganglion and its connections, check out this YouTube clip! I am not affiliated with this guy in any way, and I confess I've only listened to the first 7 minutes of the lecture, but it seems pretty good...and for those who want a more detailed description (with drawings), it's definitely worth the watch.
References and Additional Reading
- Basic and Clinical Science Course, Section 2: Fundamentals and Principles of Ophthalmology. San Francisco: American Academy of Ophthalmology, 2015.
- Kardon R. Chapter 14: Anatomy and Physiology of the Autonomic Nervous System. In: Miller NR, Newman NJ, Biousse V, Kerrison JB, eds. Walsh and Hoyt's Clinical Neuro-Ophthalmology, 6th Ed. Philadelphia: Lippincott Williams & Wilkins, 2005. pp. 673-674.
- Sinnreich Z, Nathan H. The ciliary ganglion in man. Anat Anz 1981;150: 287 – 297.
- Grimes P, von Sallmann L. Comparative anatomy of the ciliary nerves. Arch Ophthalmol 1960;64:81-91.
- Eliskova M. Blood vessels of the ciliary ganglion in man. Br J Ophthalmol 1973;57:766-772.
- Basic and Clinical Science Course, Section 5: Neuro-Ophthalmology. San Francisco: American Academy of Ophthalmology, 2015.
- Warwick R. The ocular parasympathetic nerve supply and its mesencephalic sources. J Anat 1954;88:71–93.
- Kawasaki A. Chapter 16: Disorders of Pupillary Function, Accommodation, and Lacrimation. In: Miller NR, Newman NJ, Biousse V, Kerrison JB, eds. Walsh and Hoyt's Clinical Neuro-Ophthalmology, 6th Ed. Philadelphia: Lippincott Williams & Wilkins, 2005. pp. 760-765.
- Newsome DA, Einaugler RB. Tonic pupil following retinal detachment surgery. Arch Ophthalmol 1971;86:233-234.
- Bajart AM, Robb RM. Internal ophthalmoplegia following inferior oblique myectomy: A report of three cases. Ophthalmology 1979;86:1401-1406.
- Stromberg BV, Knibbe M. Anisocoria following reduction of bilateral orbital floor fractures. Ann Plast Surg 1988;21:486-488.
- Corbett JJ, Nerad JA, Tse D, et al. Results of optic nerve sheath fenestration for pseudotumor cerebri: the lateral orbitotomy approach. Arch Ophthalmol 1988;106:1391-1397.
- Lobes LA Jr, Bourgon P. Pupillary abnormalities induced by argon laser photocoagulation. Ophthalmology 1985;92:234-236.
- Patel JI, Jenkins L, Benjamin L, et al. Dilated pupils and loss of accommodation following diode panretinal photocoagulation with sub-tenon local anaesthetic in four cases. Eye 2002;16:628-632.
- Pfeiffer N, Kommerell G. Sector palsy of the sphincter pupillae muscle after argon laser trabeculoplasty. Am J Ophthalmol 1991;111:511-512.
- O’Connor M, Eustace P. Tonic pupil and lateral rectus palsy following dental anaesthesia. Neuroophthalmology 1983;3:205-208.
- Sen DK. Isolated pupillary paralysis in a case of herpes zoster. J Pediatr Ophthalmol Strabis 1979;16:33-34.
- Rogers JW. Internal ophthalmoplegia following chickenpox. Arch Ophthalmol 1964;71:617-618.
- Sundaram MBM. Pupillary abnormalities in congenital neurosyphilis. Can J Neurol Sci 1985;12:134-135.
- Bowie EM, Givre SJ. Tonic pupil and sarcoidosis. Am J Ophthalmol 2003;135:417-419.
- Levy NS, Kramer SG, de Barros T. Pupillary and accommodative abnormalities in the Vogt-Koyanagi-Harada syndrome. Am J Ophthalmol 1970;69:582-588.
- Victor DI, Green WR, Stark WJ, et al. A non-permanent tonic pupil in rheumatoid arteritis. Can J Neurol Sci 1977;4:209-212.
- Bennett JL, Pelak VA, Mourelatos Z, et al. Acute sensorimotor polyneuropathy with tonic pupils and an abduction deficit: An unusual presentation of polyarteritis nodosa. Surv Ophthalmol 1999;43:341-344.
- Currie J, Lessell S. Tonic pupil with giant cell arteritis. Br J Ophthalmol 1984;68:135-138.
- Foroozan R, Buono LM, Savino PJ, et al. Tonic pupils from giant cell arteritis. Br J Ophthalmol 2003;87:510-512.
- Massey EW. Pupillary dysautonomia and migraine: Is Adie’s pupil caused by migraine? Headache 1981;21:143-146.
- Haider S. Tonic pupil in lymphomatoid granulomatosis. J Clin Neuroophthalmol 1993;13:38-39.
- Brooks-Kayal AR, Liu GT, Menacker SJ, et al. Tonic pupil and orbital glial-neural hamartoma in infancy. Am J Ophthalmol 1995;119:809-811.
- Monteiro MLR, Coppeto JR, Milani J. Iron mydriasis: Pupillary paresis from an occult intraocular foreign body. J Clin Neuroophthalmol 1993;13:254-257.
Did we miss anything? Do you have any other helpful hints on how to remember the different aspects of the ciliary ganglion? Leave a comment or contact us!